Supporting your employees’ full health during COVID-19
Nearly four months after the earliest quarantine orders went into effect, 72 percent of Americans surveyed said the coronavirus pandemic has been the worst time of their lives.1 Without a doubt, this has been a very and uniquely challenging time for us all—and those challenges are only going to continue for employers as more companies begin to explore return to the workplace scenarios.
While some of your employees are ready and willing to get back to the workplace, and others are going to be remote for several more months (Google announced their employees are working from home (WFH) until at least summer 2021, for example), there’s sure to be an uncommon level of stress on everyone in your organization. That’s why moving forward, we know recognizing and supporting the overall well-being of your people is job one.
THE CURRENT STATE OF THINGS

Before COVID-19, only 15 percent of Americans had paid WFH days and just over two percent worked from home five days a week. During COVID-19, that number abruptly changed: 42 percent of US employees are WFH and 33 percent are not working at all, meaning an astounding two-thirds of the US GDP is being driven by those working remotely. Post COVID-19, US firms are forecasting WFH days to be about 20 percent of all working days.2
Based on a study conducted earlier this year by Professor 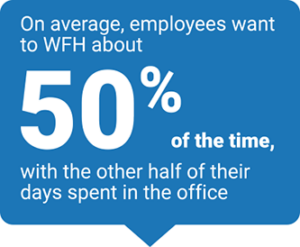 Nicholas Bloom, Department of Economics at Stanford University, employees on average want to WFH about 50 percent of the time, with the other half of their days spent in the office.3 So when it comes to WFH, there seems to be a disconnect between what firms are forecasting and employee preferences.
Nicholas Bloom, Department of Economics at Stanford University, employees on average want to WFH about 50 percent of the time, with the other half of their days spent in the office.3 So when it comes to WFH, there seems to be a disconnect between what firms are forecasting and employee preferences.
Professor Bloom’s research has shown, as many employers have seen in their own workforce, that working from home increases productivity for most workers. He highlights the presence of a ‘honeymoon’ period where these figures peak for the first three or so months before leveling off. However, WFH does have its downfalls, such as isolation, hours creep, decreased creativity, and fewer career development or growth opportunities.
Working from home during the COVID-19 pandemic has also created additional challenges, particularly for caregivers, who are struggling with balancing their jobs and the need to look after children and provide remote learning support, or caring for parents or others dealing with illness or in need of assistance. Plus, being apart has made it more difficult to engage with others and identify when team members may need additional support for both their mental and physical well-being.
Impact on physical health
A recent Blue Cross Blue Shield Association (BCBSA) National Generation Survey asked people how their activities have changed since coronavirus, and here’s what they said:
- 50 percent are eating more food and/or eating more often
- 30 percent are exercising less often
- 28 percent are drinking more alcohol and/or drinking alcohol more often
- 27 percent are sleeping less
- 15 percent are smoking cigarettes more often or started smoking
- 14 percent are taking more drugs for something other than a required medical reason
(Source: BCBSA National Generation Survey, 2020)
Impact on mental and emotional health
In that same BCBSA survey, 19 percent of people also said they’re speaking more to a therapist, counselor or mental health professional. Some contributing factors could include:
- Social isolation as a result of quarantine and being confined to small spaces
- Having to manage taking care of children and work
- Taking care of older or ill family members—e.g. millennials may have to take care of their parents and their children
- Financial concerns, such as losing a job, family members losing their jobs, being furloughed, salary reductions, etc.
- Taking less time off (vacation and sick days) to get a mental break
- Dealing with losing friends/relatives to COVID-19
- Added anxiety that comes with uncertainty
A NEW KIND OF STRESS
Whether you’re planning on bringing your workforce back full-time, part-time or in shifts, returning to the workplace could add another source of stress and anxiety for your employees. Before we can explore ways to address their concerns, let’s talk about some of the things your employees may be worried about as they return to the workplace in the COVID-19 era.
New sources of stress and anxiety for your employees could include:
- Being exposed to and contracting COVID-19, concerns for bringing it home to their family and not knowing if symptoms are just a common cold, flu or allergies
- Adjusting to the new work environment:
- Having to wear a mask while working
- Worrying about social distancing at the office
- Using public spaces like breakrooms, elevators, restrooms, cafeterias
- Commuting and taking public transportation
- Arranging for childcare with many schools moving to remote learning
- Being tested for COVID-19
- How employees who test positive will be treated by others
There’s a lot to consider and opportunities for you as an employer to create a culture of health that goes well beyond providing personal protective equipment and promoting social distancing.
For example, when the Business Group on Health (BGH) surveyed large employers asking which factors they’re including in their overall health and well-being strategy, here’s how they responded5:
- 91 percent finances
- 40 percent childcare
- 24 percent transportation
- 18 percent food access and insecurity
- 7 percent housing
PROMOTING EMPLOYEE WELLNESS

Regardless of what the future of your workplace may look like—on-site or remote—employers are becoming more mindful of the overall wellness of their staff, ensuring they feel cared for, engaged and empowered.
Taking another look at the survey conducted by BGH, we see some of the ways large employers are supporting, or planning to support, the full health of their workforce5:
![]() 36 percent indicate they will implement and/or expand their access to mental health services in 2021
36 percent indicate they will implement and/or expand their access to mental health services in 2021
![]() 43 percent added new mental health benefits or offerings to support employees working from home to ease the burden of COVID-19
43 percent added new mental health benefits or offerings to support employees working from home to ease the burden of COVID-19
![]() 88 percent offered virtual telemental health services in 2020, with an additional 3 percent planning to add in 2021
88 percent offered virtual telemental health services in 2020, with an additional 3 percent planning to add in 2021
![]() 61 percent of large employers offered virtual emotional well-being/resilience services in 2020, with an additional 4 percent planning to add in 2021
61 percent of large employers offered virtual emotional well-being/resilience services in 2020, with an additional 4 percent planning to add in 2021
“Like most companies, we are taking a long, hard look at how we support mental well-being, and are actively trying to really help our employees, even more than we have.” -Benefits Manager, Technology Company
Overall employee well-being is about a positive physical state as well as having a positive state of mind. Here are some things your organization can do to help achieve a healthy workplace culture:
![]() Connect with your employees
Connect with your employees
Understanding how your employees are feeling and what is on their mind is first and foremost. Consider creating regular, formal and informal opportunities for input. This could mean conducting surveys to get a pulse of the organization so you can develop initiatives accordingly. Company leaders and managers should also openly talk about mental health, provide options for encouragement and support, and routinely check-in with employees.
![]() Communicate early and often
Communicate early and often
Be proactive and transparent in communicating all of the ways you’re prioritizing employee safety. Also be clear on your organization’s behavioral health benefits and Employee Assistance Programs (EAP), explaining what’s available and how to utilize all of the resources with an emphasis on counseling and emotional support options. Sending periodic emails or posting reminders on your intranet can help keep everyone well informed.
![]() See the full picture
See the full picture
Expand non-medical benefits that promote your employees’ full health—from physical and behavioral to financial and beyond. Benefits include childcare, caregiving, financial coaching/planning and flexible schedules. If you have employees who used to take public transportation, parking benefits could also be examined.
<strong![]() Re-evaluate benefits
Re-evaluate benefits
Based on the challenges ahead, determine if you need to make any changes or enhancements to your organization’s benefit programs. Perhaps you’ll need to expand your EAP or include additional virtual care resources in your health plan.
![]() Introduce new tools
Introduce new tools
Consider providing employees with free access to one of the many mindfulness apps or self-guided behavioral health apps on the market. Work with your health plan provider for ideas and potential partner discounts.
![]() Take it slow and be flexible
Take it slow and be flexible
Even when more folks start to return to the workplace, things won’t be the same. Be flexible and consider a hybrid in on-site/at-home model for employees to ease back into the work environment. If only some employees are returning to the workplace, make sure you’re taking steps to keep remote employees connected through tools and technology so they don’t feel isolated.
![]() Embrace resilience training
Embrace resilience training
Consider conducting resilience training with your employees. Have an expert conduct a series of seminars or webinars and provide tools for employees to use on their own.
All in all, you want to consider how your company’s physical and remote work environments, policies and processes can impact employees’ health and well-being. Aim to build a balanced, healthy workplace culture that reduces the stigma often associated with behavioral health and minimizes unnecessary stress inducers wherever possible.
We all know the road ahead isn’t going to be easy. That’s why we’re sharing ideas, listening to employers and working with our partners to make the best of a difficult situation. For additional insights on employee wellness, click here: Building a Workplace of Health—During COVID-19 and Beyond.
© 2020 Blue Cross Blue Shield Association. All Rights Reserved. The Blue Cross Blue Shield Association is an association of independent, locally operated Blue Cross and Blue Shield companies. The information contained on this website is not intended for individuals located outside of the United States.
1 The Harris Poll, COVID-19 Consumer Research, Wave 16, June 18-20, 2020
2 U.S. Bureau of Labor Statistics
3 Stanford Study, “The Bright Future of Working From Home” 2020
4 Center for Workplace Mental Health, American Psychiatric Association Foundation, “Investing In A Mentally Healthy Workforce Is Good For Business,” 2020
5 The Business Group on Health 2021 Health Care Strategy and Plan Design Survey, May 2020